

Document Type : Original Article
Authors
1 Electrical Engineering Faculty, Najafabad Branch, Islamic Azad University, Isfahan, Iran
2 Department of Pharmacology, AshianGanoTeb Biopharmaceutical Company, Gorgan, Iran
3 Cancer Research Centre, Johns Hopkins Institute, Maryland, USA
4 Department of Basic Sciences, Faculty of Veterinary Medicine, Ardakan University, Yazd, Iran
5 Department of Veterinary Medicine, Baft Branch, Islamic Azad University, Kerman, Iran
6 Department of Anatomical Sciences, Golestan University of Medical Sciences, Gorgan, Iran
7 Sepehr Pathobiology Laboratory, Gorgan, Iran
8 Department of Urology, Alborz University of Medical Sciences, Alborz, Iran
9 Iran University of Medical Sciences, Tehran, Iran
10 Department of Pathology, AshianGanoTeb Biopharmaceutical Company, Gorgan, Iran
Abstract
Graphical Abstract
Highlights
Keywords
Main Subjects
Introduction
Cancer is a serious public health problem and the second major cause of death in the world (after cardiovascular events). Any delay in the diagnosis and treatment of any type of cancer may lead to an increase in advanced-stage disease and mortality (1). Which makes the cancer issue more serious than before. Among all, the most common cancer diagnosed in females is breast cancer, excluding melanoma (2). It is the second major cause of cancer death in females, after lung cancer (2-4). Breast cancer is divided into different subtypes according to the expression of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). These subtypes have various risk factors, with some subtypes being more strongly associated with reproductive factors than others (5). One of these subtypes is triple-negative (ER-/PR-/HER2-) disease, that is more aggressive and difficult to treat than other types of breast cancer. Triple-negative breast cancer is more likely to spread to other parts of the body and come back after treatment (6). These characteristics make the triple-negative subtype more important to study. In microarray profiling, the MDA-MB-231 cell line is associated with a triple-negative subtype. MDA-MB-231 cells are invasive and when implanted orthotopically produce xenografts that spontaneously metastasize (7). BC is the most commonly spreads to the bones, lungs, brain, and liver (8). Kidney metastasis from breast cancer is rare but has been reported (9). This study focused on the effects of human metastatic breast cancer in nude mice kidney tissue. To do this, we induced the human breast adenocarcinoma subtype MDA-MB-231 in BALB/c nude mice and then evaluated the potential biological effects of the cancer on the mice's kidneys.
Methods
This study was approved by the Tehran University of Medical Sciences’ Ethics Committee (IR.TUMS.MEDICINE.REC.1400.184). Eight female nude mice, 4 weeks old and weighing 20 grams were provided by Urology Research Center at Sina Hospital. Nude mice have no thymus and are sensitive to the conditions of unsterile, needing special care and laboratory conditions (10). The mice were housed in two clean plastic cages (18x22 x30cm) and disinfected every four days. They were fed a diet containing the necessary macronutrients, prepared by the Royan Institute in Iran, and had access to tap water. The mice were housed at the Urology Research Center Animal Laboratory for two weeks before the start of the study to adapt to the environment and reduce stress. The temperature of the room was kept at 22±2°C with humidity of 55±5%, and there was a 12-hour light/dark cycle. The mice were randomly divided into two groups:
Two weeks after the injection, tumors were visible at the injection sites. The tumors were 10 millimeters in diameter. The pathological assessment confirmed that the tumors were adenocarcinoma.
After the confirmation, the mice were housed for 1 month and weighed weekly. Tumor volumes were also measured in the intervention group weekly. After one month, all 8 mice were euthanized. Tumors were removed and evaluated. Both groups' renal parenchyma was compared pathologically for possible alterations or metastatic transformations. The samples were fixed in 10% formalin buffer. After embedding, the tissues were sliced into 5-micron-thick sections using a microtome machine. The slides were then stained with hematoxylin and eosin (H&E) and seen under an Olympus light microscope. Histopathologic surveys were performed by pathologists at the Sina Urology Research Center of Tehran University. For statistical analysis, results were shown as mean±standard deviation (SD) for quantitative variables. P-values of≤0.05 were significant. For statistical analysis, the statistical software Prism version 9 for Windows (GraphPad Software, Boston) was applied.
Results
As mentioned before, eight female nude mice weighing 20 grams at first were studied. Their weekly weights (after the confirmed intervention) are displayed in Table 1, which indicated no significant difference between the two groups (P-Value=0.293). Both groups gained more weight over time (G1:21.20±0.27gr, G2:22.14±0.19gr), but case group was heavier at all times (P-value<0.05) (Figure 1).
Table 1. Body Weight (gr)
|
Week |
1 |
2 |
3 |
4 |
Mean ± SD |
|
G1 |
21 |
21.6 |
20.9 |
21.31 |
21.20 ± 0.27 |
|
G2 |
22 |
22.43 |
21.93 |
22.19 |
22.14 ± 0.19 |

Figure 1. Weight Growth, measured in four weeks
Furthermore, tumor volume measurements in the intervention group can be seen in the following Table (Table 2).
Table 2. Tumor Volumes (mm3)
|
Case |
1st week |
2nd week |
3rd week |
4th week |
|
1 |
405 |
550 |
936 |
1267.5 |
|
2 |
405 |
665.5 |
1008 |
1352 |
|
3 |
445.5 |
600 |
864 |
1008 |
|
4 |
445.5 |
726 |
936 |
1267.5 |
|
Mean ± SD |
425.250 ± 11.691 |
635.37 ± 38.363 |
936 ± 29.394 |
1223.75 ± 74.624 |
The mean weight of the removed tumors was 2.04 grams (±0.05). Also, the mean weight of kidneys in G1 was 2.8±0.07 grams, and in G2 was 2.71±0.09 grams (P-value<0.05) (Figure 2).

Figure 2. Kidney Weight in both groups (gr)
Finally, the histopathological evaluation of renal parenchymas is shown in Figure 3.
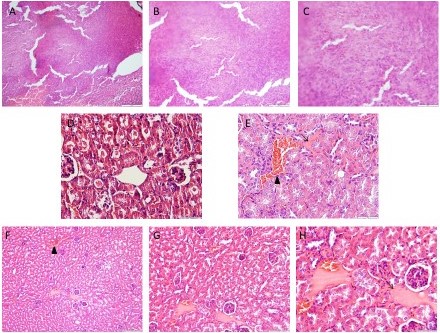
Figure 3. Histopathological sections of renal parenchyma, nude mice, H&E staining
Photomicrographs A-C shows human breast cancer (metastatic adenocarcinoma xenograft). Panels C and H (x400) show higher magnification of photomicrographs in panels B and G (x200) and these panels are higher than panels A and F (x100). Photomicrographs D and E (x400) demonstrate normal and injured structures of the kidney tissue in groups 1 and 2, respectively. The thin arrow indicates the edema and the arrow head shows the hyperemia. Photomicrographs F-H of group 2 shows no metastatic foci.
Discussion
As mentioned before, the main cause of death in famails is breast cancer (11). BC like all other cancers can metastasize to other parts of the body (12). One of the most important organs related to the breast cancer metastasis is the kidney. The presence of renal metastases can make it difficult to diagnose breast cancer, as the symptoms of kidney metastasis can be similar to the symptoms of other conditions, such as kidney stones. Additionally, the presence of kidney metastases can make it more difficult to treat breast cancer, as the cancer cells may be resistant to treatment. So, in the present study, the pathological effects of human metastatic breast cancer on nude mice kidneys were investigated.
No significant difference was shown in the weight of kidneys between the two groups at the start of this research. However, after four weeks, the mice in group 2 (G2) weighed a bit higher than the mice in group 1 (G1). The graph shows that the average renal weight of group 2 is lower than Group 1's average renal weight. This suggests that the increase in weight in group 2 may be due to the tumor growth, rather than an increase in the size of the kidneys. The increasing trend of the volume of tumors and their weight at the end of the period suggests that the disease-induced model was successful in inducing breast cancer in the mice. Despite the presence of some pathological symptoms in the kidney tissue of the second group of mice compared to the first group, such as hyperemia and edema, no evidence of metastasis of cancer cells to the kidney tissue was observed. This finding is consistent with Di Benedetto et al., study which indicated that the MDA-MB-231 cell line did not produce distant metastases including the urogenital system (13). Another study mentioned that it has been documented that metastasis to visceral organs in the animal model of triple-negative breast cancer is possible, but it is noteworthy that our research showed the absence of metastatic foci in each experimental group (14). Furthermore, other studies discussed that cancer-to-cancer metastasis such as the simultaneous or consecutive finding of a kidney tumor in females with breast cancer is a very rare phenomenon (15-19). Two comprehensive literature review articles again confirmed the rarity of breast cancer metastasis to the kidney (20, 21). These findings suggest that the injection of human metastatic breast cancer cells into the left flank region of nude mice can lead to the development of breast cancer; furthermore, metastasis of cancer cells to the kidneys does not appear to be a common occurrence.
Conclusion
Despite tissue changes and pathological evidence in the kidneys of tumor-bearing nude mice, no evidence of metastatic foci was observed in the renal parenchyma of the mentioned animals, which can somehow indicate the special feature of nude mice is not metastasizing. As a result, it can be said that the metastatic adenocarcinoma cell line of human breast cancer does not metastasize to the kidney tissue of nude mice.
Author’s contributions
AD: Data curation, formal analysis, funding acquisition, investigation, FK: Data curation, investigation, methodology, resources, LP: Methodology, project administration, resources, software, validation, AKh: Data curation, formal analysis, animal modeling, FSA: Data curation, formal analysis, animal modeling, SMD: Data curation, formal analysis, animal modeling, SGh: Animal Modeling, Validation, AS: Pathology review, BK: writing–review and editing, RGH: writing–review and editing, GhM: Conceptualization, Supervision; data curation, formal analysis, methodology, validation, visualization, writing –review and editing.
Acknowledgments
Thanks to the Urology Research Center, Tehran University of Medical Sciences, Tehran, Iran.
Conflict of Interest
The authors declare that there is no conflict of interest.
Funding
No funding.
Ethical statement
This study was approved by The Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.184).
Data Availability
No additional data are available for this editorial.
Abbreviations
ER Estrogen receptor
H&E Hematoxylin and eosin
HER2 Human epidermal growth factor receptor 2
PR Progesterone receptor
SD Standard deviation